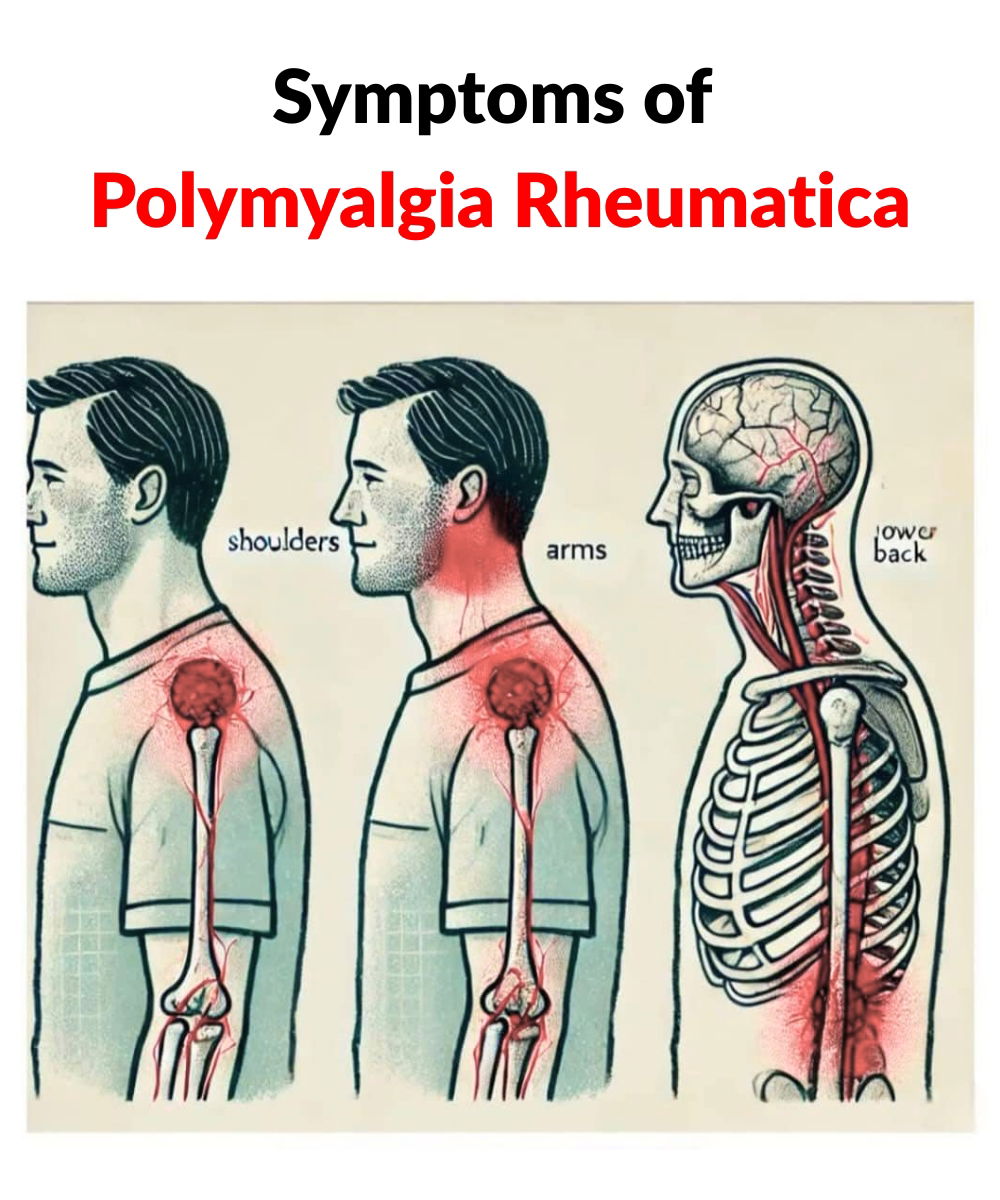
Polymyalgia rheumatica is an incendiary condition represented by muscle and joint stiffness. Happening mainly in the hips and shoulders, polymyalgia symptoms either show suddenly or gradually over several days. This condition rarely impacts individuals younger than 50 and is most popular in seniors over the age of 65. In this article, we will discover a few of the important symptoms that may suggest you have polymyalgia rheumatica.
Shoulder Pain

Polymyalgia rheumatica typically begins with aching shoulder pain. This makes displaying everyday activities, such as dressing or reaching for things, very difficult. The pain is usually shown on both sides of the body and often worsens at night, making it hard to sleep.
Neck, Buttock, Thigh, Hip, and Upper Arm Pain

While the pain typically begins in the shoulders, many people also deal with pain in other major muscle groups, such as those found in the hips, upper arms, buttocks, thighs, and neck. This deep pain often gets worse after doing tasks that demand repetitive movement or after not being active for an extended period of time.
Stiffness

One major sign of polymyalgia rheumatica is feeling very inflexible, especially in the mornings or after being inactive for a while. Even just sitting in the same position for a while can affect parts of the body to stiffen up, which makes moving very uncomfortable.
Limited Range of Motion
If left uncured, the stiffness can cause a limited range of motion. For example, your shoulders aching if you try and move them beyond a certain range, making it difficult to raise your arms upwards or extend them outward. It can also cause weakened hip mobility, making activities such as getting up from a seated position or climbing stairs difficult.
Knee, Elbow, and Wrist Pain

While most people mostly deal with pain in their hips and shoulders, some people also suffer from stiffness in their knees, elbows, and wrists. Writing or typing becomes very challenging due to the wrist pain, and even walking can become a struggle because of the effect of the knee pain.
The Bottom Line
As we grow older, our bodies become more vulnerable to various conditions. These conditions often cause limitations to our movement because of the pain. Many polymyalgia rheumatica patients deal with stiffness and pain that drastically affect their mobility, making performing everyday tasks a real struggle. If you see any of these signs in your or a loved one’s daily life, it’s best to consult a health practitioner.
5 W𝓪rning Signs of Psoriasis You Shouldn’t Ignore

Explore the key symptoms of psoriasis, its causes, and treatments. Learn when to consult a doctor for this chronic skin condition.
Psoriasis is a chronic skin condition that affects millions of people in the world. Though it’s not contagious, it’s essential to recognize its symptoms early to manage the condition effectively. Below’s what you need to know about the different types of psoriasis, their causes, and how to seek the right treatment.

Psoriasis manifests in a variety of forms, each with distinct characteristics:
Plaque Psoriasis: The most common type, presenting as red patches of skin covered with silvery scales.
Guttate Psoriasis: Identified by small, drop-shaped spots, often triggered by infections like strep throat.
Pustular Psoriasis: Marked by red, inflamed skin topped with pus-filled blisters.
Inverse Psoriasis: Appears in moist areas like skin folds, leading to shiny, red lesions.
Erythrodermic Psoriasis: A rare and severe form that causes widespread redness, peeling, and a burning sensation—this is a medical emergency requiring immediate attention.

Psoriasis occurs because of an immune system malfunction where T-cells mistakenly attack healthy skin cells, leading to rapid skin cell turnover. Genetic factors play a significant role, and certain triggers can exacerbate the condition, including:
– Excessive alcohol consumption
– Infections
– Specific medications, like beta-blockers or lithium

A dermatologist typically diagnoses psoriasis through a physical exam, though a skin biopsy might be necessary in some cases. While there’s no cure for psoriasis, several treatments can help manage symptoms and improve quality of life:
Topical treatments: Corticosteroids and vitamin D analogs.
Phototherapy: Controlled exposure to ultraviolet light.
Systemic treatments: Oral or injectable medications for severe cases.
If you notice persistent skin issues like red patches, scaling, or unusual rashes, it’s crucial to consult a doctor. Early diagnosis and treatment can prevent complications and significantly enhance your quality of life.
Understanding psoriasis and its triggers empowers you to take control of your skin health. Don’t ignore the signs—seek medical advice to stay ahead of this condition.